On Friday, March 13, President Donald Trump and Vice President Mike Pence stood in the White House Rose Garden to declare COVID-19 a national emergency. But the risk of the disease, Pence told the nation, remained low.
“We don’t want everybody taking this test; it’s totally unnecessary,” Trump assured Americans. “This will pass.”
About 1,000 miles south of Washington, as if heeding their call, thousands of spring breakers had converged on Miami Beach. They played tug of war on the sand and snapped selfies by the water.
“If I get corona, I get corona,” one tourist from Ohio told reporters. “At the end of the day, I’m not gonna let it stop me from partying.” For them, the specter of the COVID-19 pandemic seemed very far away.
Like Trump, Florida’s Republican governor, Ron DeSantis, had downplayed the threat of COVID-19. Just a few days earlier, when Dr. Anthony Fauci, the nation’s leading expert on the pandemic, had said Florida was experiencing community spread of the virus, DeSantis had retorted that it wasn’t true. The governor also had balked at closing the state’s beaches to check the virus’s spread.
That weekend after Trump’s address, Miami Beach Mayor Dan Gelber took a stroll on Ocean Drive, a thoroughfare lined with palm trees and historic Art Deco buildings. He came to a sudden realization that not one person out of the thousands he saw was practicing social distancing. Without widespread testing, he thought, the virus could be silently spreading through his city.
It hit Gelber: He had to close the beach.

“At that point, I realized that I was not going to rely on the federal government to tell us what to do,” he said. “I obviously couldn’t rely on the state.”

Across the country, Dr. Scott Morrow was experiencing his own day of dread. The veteran public health officer for San Mateo County, on California’s San Francisco Peninsula, Morrow had no proof that the virus was spreading. Medical testing supplies were maddeningly impossible to come by. But he had become convinced that the potentially deadly virus, which had first been noted in the area only six weeks before, was “spreading like wildfire under our noses.”
Morrow feared that the entire San Francisco Bay Area, a region of more than 7 million people, would soon be “following Italy into the abyss,” with an exponential growth curve of infection and death.

Worse, Morrow was running out of ideas for checking the contagion. Already, he had banned large public gatherings. The county’s schools were shutting down. Deeply frustrated, he recalled sending an email to county officials, warning them, “This is all I can do – I’m out of options.”
On a rainy Sunday morning two days later, Morrow was awoken by a text message: Would he jump on a call with Dr. Tomás Aragón, the public health officer in San Francisco, and Dr. Sara Cody, the health officer of Santa Clara County in the hard-hit Silicon Valley?
In a day of calls that soon included county counsel, the officers converged on a radical consensus – to use their broad powers under California public health law in a way that had never been tried in the United States. To stop the spread of the disease, they would order the public to stay in their homes and shelter in place.

“This is what needed to be done,” Morrow said. Bay Area health officers announced vast shutdown orders the next day.
Morrow recalls feeling “scared shitless.” Would the public comply with shelter in place? And even if they did, would it work?
A week and a half later, on March 26, the U.S. became the global epicenter of the COVID-19 pandemic.
Blunting the pandemic
At a congressional hearing in mid-May, a recently ousted federal health official pulled back the curtain on the colossal missteps that had undercut the federal response to the pandemic. Rick Bright had filed a whistleblower complaint charging that he was removed from his post as the deputy assistant secretary for preparedness and response at the Department of Health and Human Services when he urged the vetting of hydroxychloroquine, the anti-malaria drug Trump touted as a cure for COVID-19.
Bright testified that he and several colleagues had warned the White House as early as January that the country was unprepared for a pandemic.
“We knew going into this pandemic that critical medical equipment would be in short supply,” he told Congress on May 14. “I was met with indifference, saying they were either too busy, they didn’t have a plan, they didn’t know who was responsible for procuring those.” The federal government not only had failed to secure critical supplies, such as ventilator masks and testing swabs, he said, but had failed to provide clear guidance to the nation.

“Our population is being paralyzed by fear,” he said, “stemming from a lack of a coordinated response and a dearth of accurate, clear communication about the path forward.”
The testing shortages, in particular, hampered public health officials as they tried to confront the looming threat, said Dr. John Swartzberg, an epidemiologist with the joint medical program of the University of California, Berkeley and UC San Francisco. For epidemiologists, tests are “our eyes” in a pandemic, Swartzberg said, and the rollout was so badly botched that decision-makers were left in the dark.
At first, testing was delayed because the Centers for Disease Control and Prevention chose to create its own test rather than partner with private labs. When the new CDC tests were finally ready, the agency failed to ramp up production – and the tests themselves had technical defects. State labs had to send their samples to CDC headquarters in Atlanta, causing a long backlog.
“States can do their own testing,” Trump would later say. “We’re the federal government. We’re not supposed to stand on street corners doing testing.”
Response to the pandemic in the global epicenter would be left to states and cities.
The earliest states to be hit by the pandemic would face the toughest tests, forced to consider unprecedented decisions. Among the first states with confirmed cases – and confirmed deaths – were California and Florida, whose governors’ wildly different leadership styles influenced the states’ responses.
California Gov. Gavin Newsom, a Democrat, ultimately followed the lead of local health officers and became the first in the nation to extend shelter-in-place orders to the entire state.
In Florida, Gov. Ron DeSantis, a Republican, issued only vague recommendations until late in the game, leaving local governments in charge of crucial decisions. He refused to close all of the state’s beaches and delayed issuing a statewide stay-at-home order for weeks, until 36 states had already done so and Florida had surpassed 100 deaths. In a statement to Reveal from The Center for Investigative Reporting, DeSantis spokesperson Cody McCloud said “the Governor’s Office worked with these mayors to ensure the needs of their counties were being met” as they made decisions early on in the pandemic.
Nowhere was the federal government’s scattershot response to the pandemic – and the contrast between the two governors – on more vivid display than in the distinct fates of cruise ship outbreaks that ended up in California and Florida ports.
The California-bound liner, the 3,500-passenger Grand Princess, had one COVID-19 death and nearly two dozen other cases by the time it approached San Francisco Bay in early March. Trump had made clear that he wasn’t keen on the ship coming ashore, concerned it would inflate the nation’s COVID-19 caseload.

“I like the numbers being where they are,” he said March 6. “I don’t need to have the numbers double because of one ship that wasn’t our fault.”
Newsom feared that if the ship docked in San Francisco, infection might sweep through the city. After prolonged consultations with the CDC, Pence’s coronavirus task force and other federal health officials, Newsom announced a plan: The Grand Princess would dock in Oakland, and U.S. passengers would be put into quarantine at a cluster of military bases.
Florida’s cruise ship crisis involved 1,200 passengers on two Holland America liners, the Zaandam and the Rotterdam. Some 150 passengers had developed flu-like symptoms by the time Port Everglades became the ships’ last resort.
Here, DeSantis left decision-making in the hands of a unified command of eight local and federal agencies. That team, as in California, included the CDC. But the outcome could not have been more different.
On April 2, when the ships were allowed to dock, 13 seriously ill passengers and one crew member were taken to hospitals. Without being tested or quarantined, the other passengers headed for the airport, where they boarded chartered flights to such major cities as Atlanta, Toronto, London – and San Francisco.
The distinct pandemic responses in California and Florida were also shaped by the two states’ vastly different health infrastructures. While in California, counties have independent and highly autonomous health officers, Florida has a more centralized health department with branch offices in each county. The department largely takes orders from the governor. If the state’s leadership is slow, so is the department’s response.
Florida Department of Health officials declined an interview to discuss their pandemic response, noting in a statement only that their approach has been “strategic and methodical.”
Reveal, in partnership with KQED in San Francisco and WLRN Public Media of South Florida, interviewed dozens of elected officials, public health officers, mayors, hospital directors and educators to provide an unprecedented look at how key decisions made by local officials ultimately saved lives as the Trump administration downplayed the threat of the virus in the early days of the pandemic.
California’s governor had feared millions of coronavirus infections. Instead, the state’s case rate fell below the national average, and the death toll, according to information compiled by the CDC and the Institute for Health Metrics Evaluation at the University of Washington, was far lower than initially feared.
Florida also skirted the early disaster that some experts had feared. By late March, Florida’s case rate began to overtake California’s, but the state’s hospital system was never overwhelmed.
Bold action by local officials appears to have blunted the force of the pandemic in those crucial early weeks.
Chinatown
California’s first case – and the nation’s third – was confirmed Jan. 25, when an Orange County man who had recently traveled to Wuhan, China, was hospitalized. But experts now believe that COVID-19 likely established itself weeks earlier.
That’s when Jian Zhang, CEO of the Chinese Hospital in San Francisco’s Chinatown, began to sense that the viral outbreak in Wuhan was building into a pandemic that would inevitably spread to the West Coast.
Trump, in his first public comment on the novel virus, had dismissed concerns, saying: “It’s one person coming in from China, and we have it under control. It’s going to be just fine.”
But Zhang said she was alarmed by word from an old medical school classmate that a volunteer Chinese medical team was flying three hours to Wuhan before the Jan. 25 start of the Lunar New Year, China’s biggest holiday. “When you deploy a team like that and you have to leave on Chinese New Year’s Eve,” Zhang recalled thinking, “something must be really serious.”

The outbreak was coming at a dangerous time. The Lunar New Year marks the largest human migration on earth, as hundreds of millions travel to visit family for the extended holiday. And Zhang knew there was direct air service between Wuhan and San Francisco.
“I’m like, my God, it’s only 12 hours away,” she said.
Zhang decided to stock up on protective equipment for the hospital, including 2,000 ventilator masks. But the masks were back-ordered. She phoned the local official who represents Chinatown on the Board of Supervisors, Aaron Peskin.
“This will be a nightmare of yours and mine if we have the outbreak in Chinatown,” she told him. Zhang and Peskin pulled together a news conference Feb. 1 to warn of the coronavirus threat and urge Chinatown residents to reduce their risk of infection. Wash your hands, they repeated.
Meanwhile in Florida, a hospital just outside Fort Lauderdale was having its first brush with COVID-19. A woman visiting from a province near Wuhan showed up at a Memorial Healthcare System hospital with flu symptoms, sparking a flurry of local coverage. She tested negative for COVID-19, but the incident was a wake-up call, prompting the hospital to dust off its pandemic preparedness plan.
“My chief of infectious disease and my chief epidemiologist basically said that this will come,” said Chief Medical Officer Dr. Stanley Marks. “This will be a pandemic.”
Eerie days
For Dr. Sara Cody, health officer in California’s Santa Clara County, the weeks before COVID-19 were like driving in a dense fog. You knew there might be a cliff around the bend. But you couldn’t see it.
In January, she and her staff started reading up about “some unusual virus that was emerging in China,” she said in an interview. Whatever the virus turned out to be, Cody thought it was headed her way: There’s a tremendous amount of routine air travel between Silicon Valley and Asia.
“So I was thinking, you know, it’s likely we’re going to see this early,” she said.
By Feb. 3, Santa Clara County, home to San Jose, had confirmed two cases of COVID-19: Both patients had traveled to Wuhan. Cody declared a local public health emergency.
“And then,” she recalled, “we had this eerie February, where we had no more cases reported, no more cases detected.”
As the weeks passed, Cody made reassuring public statements about COVID-19, to the point that some local officials complained that she was downplaying the risk. At one meeting, on Feb. 19, she said, “We don’t have any evidence still to date that the coronavirus is circulating in our county.”

But behind the scenes, she was scrambling to track the virus’s spread. A health officer’s playbook for containing a pandemic begins with aggressive testing. In the case of COVID-19, the supply of tests was grossly inadequate – and the tests themselves were unreliable.
Throughout February, Cody said her staff was desperately trying to run the new CDC tests in local laboratories, but they couldn’t make them work. So every sample had to be sent to the CDC for testing, and “there was this huge, long process to get a specimen to the CDC and get it back,” she said.
“And so the month of February was just strange, because you had the sense that probably something might be going on, but we didn’t know what it was.”
On Feb. 27, Dr. Scott Morrow of neighboring San Mateo County, Cody’s longtime colleague, wrote an extraordinarily blunt letter to the county’s 700,000 residents.
COVID-19 might become “a severe pandemic,” read the letter, posted on the county’s website. Everyone’s lives might be “significantly disrupted.”
He ticked off a series of orders that might become necessary: social distancing. A ban on gatherings. Closing schools. Rationing critical supplies.
“This is a difficult message to share,” he wrote, “but it is important to recognize how difficult the times ahead may be.”
In Florida, February was an extraordinarily quiet month when it came to the emerging world pandemic.
One of the first public rumblings about the virus came from the governor at a Feb. 27 news conference. DeSantis said there were no confirmed cases of COVID-19 in the state, then evaded questions from reporters about how many people had actually been tested.
“I don’t think I’m allowed to go into the numbers,” he said, citing a state law that protects medical information of people undergoing “epidemiological investigations.”
But legal experts and lawmakers were quick to point out that the law allowed the state to share aggregate numbers during a public health crisis. “It was a complete firewall of information,” said state Sen. Jose Javier Rodriguez, a Miami Democrat. “They say they can’t, when in reality they won’t.”
While Rodriguez was in Tallahassee for the legislative session, he asked for a meeting with the state Department of Health to discuss COVID-19 testing and preparedness. Medical experts were already encouraging elbow bumps in lieu of handshakes to prevent infection. So he was stunned when the health officials arrived at his office and one tried to shake his hand.
“I really did feel like Chicken Little,” Rodriguez said. “This is a real thing. They’re not telling us if it’s here or if it’s coming. And the first person at the first meeting I’m having about this is trying to shake my hand. And I was like, what’s going on?”
Within days, on March 1, DeSantis confirmed the state’s first two cases.
California steps in
From the start, Gov. Gavin Newsom was the telegenic face of California’s fight against the pandemic. His earnest, information-packed press conferences, some lasting as long as an hour, were live-streamed and often dominated local evening news.
Californians liked what they saw: By April, Newsom’s approval rating had increased by an astonishing 41 points, to 83%, FiveThirtyEight reported. After he made an appearance on Rachel Maddow’s MSNBC show, the hashtag #PresidentNewsom briefly trended on Twitter.
There were missteps: Newsom was slow to acknowledge problems with COVID-19 testing – at one point, California had a backlog of 60,000 tests, reportedly the worst in the country — and for a time, like Trump, he insisted, despite all evidence, that testing was readily available. (Newsom later acknowledged a problem – “I own that,” he said – and promised to improve.)
Yet the governor took action only after local officials had cleared the way. That first became apparent in connection with one of his earliest attempts to check the virus – the March 11 ban on large gatherings.

As COVID-19 gathered steam in the early days of March, health officers in the Bay Area started rolling out strategies to disrupt its spread. At first, this amounted only to strongly worded guidance.
In a March 5 letter, Dr. Scott Morrow urged San Mateo County residents to practice social distancing and cancel nonessential gatherings. “This is not business as usual,” he wrote.
The following day, San Francisco Mayor London Breed issued her own recommendations discouraging large gatherings. In Santa Clara County, Dr. Sara Cody did the same.
Across Silicon Valley, the giants of the tech industry responded in force, asking tens of thousands of employees to work from home. Among them were such powerhouses as Facebook, Google, Apple, Twitter, Salesforce and LinkedIn.
But as the health officers learned, not every business was willing to voluntarily follow suit.
San Jose’s NHL team, the Sharks, and San Francisco’s NBA team, the Golden State Warriors, both continued to play games – potentially allowing the virus to spread among their thousands of fans.
Playing those games was “the worst thing you could do in the face of the pandemic,” said Dr. John Swartzberg, the UC epidemiologist.
The health officers countered by issuing orders banning large gatherings altogether, shutting the sports teams down.
It was two days after Santa Clara announced its ban that Newsom followed suit by issuing one statewide. That became the pattern: Local officials would issue tough orders, and the governor would expand on what they did. On the difficult matter of closing public schools, for example, educators said the governor flatly refused to take the lead.
Experts knew that public schools were a potential breeding ground for the virus. One infected child could pass on the virus to dozens of classmates, teachers and family members. Closing schools was an obvious way to limit viral transmission.
But officials also recognized that school closings would send a ripple of pain through every community. Working families would have to arrange child care or give up jobs. Grandparents – among the most vulnerable to serious illness from COVID-19 – would wind up taking care of kids. The logistics of reaching families in need of school meal programs would be formidable.
For a while, the downside of closing schools outweighed the benefits, as Cody put it. But early in March, starting with Elk Grove in suburban Sacramento, individual districts in California began to close schools when students or parents were diagnosed with COVID-19. In San Francisco, Superintendent Vincent Matthews shut down 2,900-student Lowell High School.
Visit TextFancy.com to make your strings more stylish. Pick emojis and other characters, generate ascii art and more.
On Monday, March 9, the governor met with school superintendents in the State Capitol. Matthews drove the 90 miles to Sacramento, he recalled, “to find out whether he was going to close schools or not.”
Newsom wouldn’t do it.
“He was emphatic about that,” Matthews said, “that he was not going to close schools. He just said it was a local decision and he was going to let local districts make the call.”
Back in San Francisco, Matthews decided to act swiftly. He consulted the county health officer, Dr. Tomás Aragón, and held an emergency meeting of the school board. On Thursday, March 12, he announced that all schools in his district would close. “We just determined that, you know, we needed to slow things down,” Matthews said.
The following day, a wave of other districts – including Los Angeles, with more than 700,000 students – followed San Francisco and shut down schools. Only then did the governor issue an order guaranteeing that districts that closed because of the pandemic would still receive state funding.
As life in California was grinding to a halt, Florida’s social and political life mostly went on undisturbed. In early March, state lawmakers still greeted each other with bear hugs in the State Capitol. Tourists still crowded Disney World and Universal Studios. The Winter Party Festival, an annual LGBTQ event in Miami Beach, drew thousands of partygoers, some of whom later died of COVID-19.
But slowly, the first signs of a disturbance to Florida life emerged. Miami officials postponed the electronic dance music event Ultra Music Festival, despite protests by ticket holders on social media. As Florida’s presidential primary neared, older poll workers concerned about getting exposed to the virus started to drop out, local elections officials said.
“We began receiving calls from people saying, ‘I’m not going to show up,’ ” said Peter Antonacci, Broward County’s elections supervisor. “ ‘I'm afraid of the virus.’ So we knew then that we had an issue.”
In the absence of guidance from federal and state officials, some local businesses took their own steps to protect their customers. Ruth Ann Bradley, who runs a yoga studio in Cooper City, near Fort Lauderdale, had been concerned about COVID-19 for days. She’d followed along on Facebook as yoga studios in California were closing.
She began extra cleaning precautions in early March. She and her students wiped down their yoga mats and she steam-cleaned props between classes. She encouraged everyone to use hand sanitizer and wash their hands frequently.
It was only a matter of time, Bradley thought, before the virus swept across South Florida.
Shelter in place
By Friday, March 13, the lives of millions of Californians had been disrupted to fight the pandemic. But the virus’s spread still seemed to be accelerating, and San Mateo County’s Dr. Scott Morrow began to fear that the Bay Area might be “only one or two weeks behind Italy.” There, the surge in COVID-19 cases had overwhelmed the nation’s health care system – and its morgues.
More needed to be done, Morrow believed. But as a local health officer battling a worldwide pandemic, he was “out of options,” as he wrote to county officials. Further measures would have to come from the state or federal government.
In San Francisco, Mayor London Breed said she too had concluded that more drastic action was needed: Her city of nearly 900,000 people would have to shut down.
“I felt strongly that the sooner we get there, the faster we can hopefully get out of there,” she said.
Over that weekend, Breed said she “reached out to the governor,” telling him that shutting down the city was “what we need to do.” Newsom “didn’t want me to go out there and do it on my own,” Breed said. “He wanted us to collaborate.”
And so on Sunday, Breed’s health officer, Aragón, got on the phone with his counterparts Cody and Morrow.

Bay Area health officers had been collaborating on regional health crises since the AIDS epidemic in the 1980s. They knew that state laws allow them to “take any action that you need to take to stop disease,” as Morrow put it. “They’re kind of brilliantly written. They kind of take politics out of the mix.” At one time or another, all had used those broad powers. But typically, the target was one person – a tuberculosis patient who needed to be quarantined, for example. Now, the officers were contemplating an order quarantining an entire region – both the healthy and the sick.
Like COVID-19 itself, their discussion moved rapidly. Only two days before, when Cody had banned large gatherings in Silicon Valley, the order had struck her as “so monumental and so difficult and having such profound impact,” she said.
“Never did I imagine that 48 hours later, I would have come as far as thinking that we actually needed to completely shut things down and shelter in place.”
Morrow called the process “otherworldly, literally otherworldly. … It did not seem in the realms of this world.” But somehow, by that evening, they had crafted the unprecedented shelter-in-place order. Health officers from four other counties signed on.
It’s striking how absent state officials were from the deliberations. Morrow said none of the health officials alerted Gov. Gavin Newsom or other elected officials and their input was not sought. Cody said she couldn’t remember distinctly, but thought that somebody must have at least looped in the governor via the state health department. Only Breed recalled telling the governor of her plan to lock down San Francisco; by her account, he preferred joint action by local officials. The governor’s office declined to comment for this story.
The health officers of six counties announced shelter in place that Monday, March 16, at a joint news conference in the city of Santa Clara. Breed announced San Francisco’s closure herself.
“They said they don’t want to put politics in it, but that’s wrong,” Breed said of the county health officers. “The fact is they put forward directives and then … we have to go out there and defend their orders and explain.”
Their actions may not have been coordinated with the governor, but they appear to have sent a message.
Two days later, Newsom appeared deeply worried about COVID-19. He wrote a letter to Trump, saying the state projected that 25.5 million Californians could become infected with the virus over the next eight weeks – a startlingly high figure that implied hundreds of thousands might die. Newsom’s aides later walked back the number, calling it a worst-case scenario that didn’t factor in efforts to fight the pandemic.
At the same time, California mayors – including Eric Garcetti of Los Angeles and Sam Liccardo of San Jose – were urgently lobbying the governor for a statewide shelter-in-place order. “If we didn’t have a uniform set of rules, then we would all just have our communities getting reinfected,” Liccardo said.

On March 19, two days after the Bay Area shutdown orders went into effect, Newsom extended them to the entire state. Effective immediately, nearly 40 million residents were ordered to stay at home except when conducting essential business.
California, with 19 confirmed deaths, was the first state to take this drastic measure. Without the ability to test and trace, it was arguably the only effective means of checking the spread of the pandemic. Over the next four days, eight other states shut down. Florida held off 15 more days, until April 3, when it became the 37th state to mandate shelter in place.
Florida Gov. Ron DeSantis said he was taking his lead from the White House: “It makes sense to make this move now. I did consult with folks in the White House about it. I did talk to the president about it.”
Trump had long insisted that the nation would be back to normal by Easter; by the end of March, he finally conceded that was “just an aspiration” after extending federal COVID-19 guidelines, which encouraged older people and those who feel sick to stay home, for another 30 days. DeSantis called that decision a “national pause button.”
‘Don’t wait for it to get worse’
With contradictory signals coming from Washington, all eyes were on California.
After San Francisco announced its shelter-in-place order, Breed recalls telling several mayors that they should shut down their cities. “At the time, people probably thought I was overreacting just a little bit,” she said.
City of Miami Mayor Francis Suarez was one of the mayors who immediately got on the phone with Breed in mid-March. The two are close, and Suarez took her advice seriously. He wanted to issue a shelter-in-place order in Miami, but the path forward was less clear than in the Bay Area, where the health officers enjoy extraordinary autonomy. Miami’s city attorney didn’t think Suarez or the city manager had the legal power to do it.
“We had to put a lot of internal pressure on our city attorney with our commissioners to get her to agree to it,” Suarez said.
In Fort Lauderdale, 30 miles north of Miami, City Manager Chris Lagerbloom also was in touch with his counterparts in California. They had been grappling with the virus for longer. Lagerbloom asked them: What do you wish you knew at our stage in the game?
“The answer was a resounding, ‘Don’t wait for it to get worse before you decide to take action,’ ” he said. “It was one of those times where that sank in.”
DeSantis was not yet ready to hit pause. He insisted on going forward with the state’s March 17 presidential primary. “We’re definitely voting. They voted during the Civil War,” DeSantis said at the time. Canceling it, he said, “would have really sent a signal about panic. And I don’t think that’s the signal that you want to send.”
And although he recommended postponing or canceling mass gatherings, he didn’t issue orders to ban them outright. By the second weekend of March, business and political leaders began to shut down South Florida. Miami-Dade County officials canceled the annual Youth Fair hours before it was scheduled to open. Organizers of the Firestone Grand Prix in southwest Florida postponed the race. Disney shut down its parks. At Magic Kingdom, Mickey Mouse and a menagerie of other Disney characters waved at the crowds one last time before the park shut its massive gates.
School districts, following California, began shutting down. “We started paying attention to it when (COVID-19) impacted the West Coast in particular,” said Broward County Superintendent Robert Runcie.
Runcie and his deputies met regularly to go over the district’s COVID-19 preparedness plan starting in February. Beyond protecting his staff and students, Runcie realized that he would need to coordinate any school closures with other South Florida superintendents. What happened in his district would inevitably affect neighboring ones, because many Broward County residents worked at Miami-Dade schools and some Broward school employees lived in Palm Beach County. The three superintendents began to confer, Runcie said.
“We’re all connected,” Runcie said. “So you make a decision in one district, it’s going to have ramifications in the other.”
On Friday, March 13, all three districts announced they would close schools.
But on the beach, spring break raged on through the weekend – until the Miami Beach and Fort Lauderdale mayors took the extraordinary step on Sunday afternoon of announcing that their beaches would close.
Florida is known to shut down beaches for one reason: a hurricane. Daniel Stermer, mayor of Weston and then-president of the Broward League of Cities, said he was blindsided by Fort Lauderdale’s move.
“The rest of us sort of went, ‘What did you just do? You didn’t discuss that with us,’ ” Stermer said.
As Miami Beach and Fort Lauderdale beaches emptied out, nearby coastal mayors scrambled to impose their own closures as spring breakers searched for new places to party.

In Key Biscayne, Mayor Michael Davey quickly noticed a rush on the grocery stores in his beach town.
“They’re obviously going to the beach,” he said. “They’re in bathing suits and they’re getting their beer and they’re getting their hot dogs and they're getting all their stuff and they’re buying the coolers. And I’m saying, ‘Well, this isn’t good.’ ”
Key Biscayne soon closed its beaches. So did Hollywood, where Mayor Josh Levy anticipated that spring breakers would descend on his city. “We needed to take decisive and immediate action,” he said.
For his part, the governor continued his hands-off approach. He banned gatherings larger than 10 people at beaches, but left much of the rest up to local governments. A DeSantis spokesman told Reveal that beaches weren’t closed statewide “because a one-size-fits-all approach was not the right model for Florida.”
“If you have a mother just walking down the beach with her daughter, I think that can be done safely,” DeSantis said. “That is much different than doing a Jell-O shot off somebody’s stomach.”
Looking back, Dan Gelber, Miami Beach’s mayor, said beaches should have closed sooner. The COVID-19 numbers may have been low, but who knew what that meant without widespread testing. The virus had likely already spread undetected. Miami Beach was the first to close its beach, he said, “and still, we were very late.”
Cascade of orders
After the beach closures came a wave of aggressive local action, as cities and towns across South Florida issued stay-at-home orders.
In Broward, officials from the county’s 31 municipalities scrambled to coordinate their orders, said Chris Lagerbloom, the Fort Lauderdale city manager. He was among three city managers who joined forces to draft a list of recommendations and deliver them to the rest of the cities.
Local leaders went their own way on some issues. Some instituted their own curfews. Others classified active construction projects as essential businesses. But all ultimately came out with stay-at-home orders of their own.
“It was really neat to watch,” Lagerbloom said, “because I didn’t think it was possible.”
After several cities had issued their orders, Miami-Dade and Broward counties told residents to stay home March 26.

Some residents had already taken action. At her Cooper City yoga studio, in Broward County, Ruth Ann Bradley said she felt exhausted from disinfecting her entire studio after each class. She worried about the safety of her students. Her larger classes could accommodate up to 20 at a time.
“I just kind of saw the writing on the wall,” Bradley said. “I can't go through another week of all this cleaning if I'm basically going to be closing anyway. And it just seemed like the right thing to do.”
On March 15, a week before Broward County issued its order closing nonessential businesses, she sent a notice to her students: The studio would close, and classes would be offered via Zoom.
A Tampa Bay Times analysis of cellphone tracking data found that Bradley was not alone: In every county in the state, people had begun staying home well before county and state orders were issued. By the time the governor finally ordered residents to stay home, nearly half of the state’s counties had already seen a 50% decline in activity.
DeSantis, who had been loath to intervene early on, issued a series of orders in March, ordering international travelers to self-quarantine, discouraging mass gatherings and barring visitors from nursing homes. He also ordered 1 million doses of hydroxychloroquine following Trump’s praise of the anti-malaria drug as a treatment for COVID-19. (Studies later established that it was dangerous for COVID-19 patients.)
But DeSantis rebuffed calls for a statewide stay-at-home order, arguing that a uniform approach wouldn’t be appropriate, given that some counties had very few cases.
“You simply cannot lock down our society indefinitely with no end in sight,” he said at a March 23 press conference. “And when people say that we may do this for seven to nine months, I can tell you that is not sustainable. That is not something that this society would accept.”

When his stay-at-home order landed April 1, the 34-page executive order listed religious services as essential and thus exempt from the shutdown. Two Broward County mayors, Weston’s Daniel Stermer and city of Sunrise Mayor Michael Ryan, fired off emails to DeSantis’ office asking the governor to reconsider. “Based upon proven science, these large gatherings are jeopardizing the health, safety and welfare,” Ryan wrote. “As a result, we feel very strongly not only can we restrict access, we have an obligation to do so based upon the science.”
Joe Jacquot, the governor’s general counsel, responded that DeSantis’ order allowed cities to restrict churches if they chose. Ryan wasn’t satisfied. The order, he wrote, “explicitly invalidates our local orders. We are going to run into conflict with those who do not want to comply.” A subsequent email exchange indicates that Stermer’s city attorney would call Jacquot to talk things through.
By the time the state order went into effect, Florida’s reported coronavirus death toll had topped 100.
Flattening the curve
At first, it was not at all clear whether Californians would comply with Gov. Gavin Newsom’s pathbreaking shelter-in-place order. The weekend after it went into effect, Venice Beach in Los Angeles was mobbed, and the governor was irked.
“Those young people are still out there on the beaches thinking it’s time to party,” Newsom said at a news conference. “It’s time to grow up.”
The normally secluded beaches of San Mateo County, south of San Francisco, “looked like Waikiki,” complained Dr. Scott Morrow, the county health officer. And he had noticed other signs of noncompliance – large picnics and outdoor sports. Morrow called out the scofflaws.
“If you decide you want to do your own thing and follow your own rules, you disrespect us all,” he wrote in an open letter. “You spit in our face, and you will contribute to the death toll that will follow.”
As days passed, compliance improved. The experts’ worst fears – that, like Italy, California’s hospitals would be overwhelmed with gravely ill patients – had been staved off, for now.
“What I mostly remember from those weeks is racing around trying to find out, you know, where we can stand up alternate care sites,” said Santa Clara County’s Dr. Sara Cody, referring to temporary facilities that could house patients once Bay Area hospitals were full.
“We were imagining ICUs that were going to be brimming,” she said. “We had our mass fatality plans reviewed and revised. And then, of course, our shelter in place helped to really slow things down. And our hospitals never saw that surge.”
Newsom’s statewide shutdown order appears to have gotten traction: In the weeks that followed, California suffered far less from the pandemic than other states, with both case rates and death rates below the national average, despite the state having been host to the first confirmed case of community transmission.
Testing data also suggests the profound impact of those early Bay Area shelter-in-place orders: The Bay Area’s curve flattened quickly and dramatically after the shutdown and continued to plateau even as the number of COVID-19 cases in the rest of the state rose.
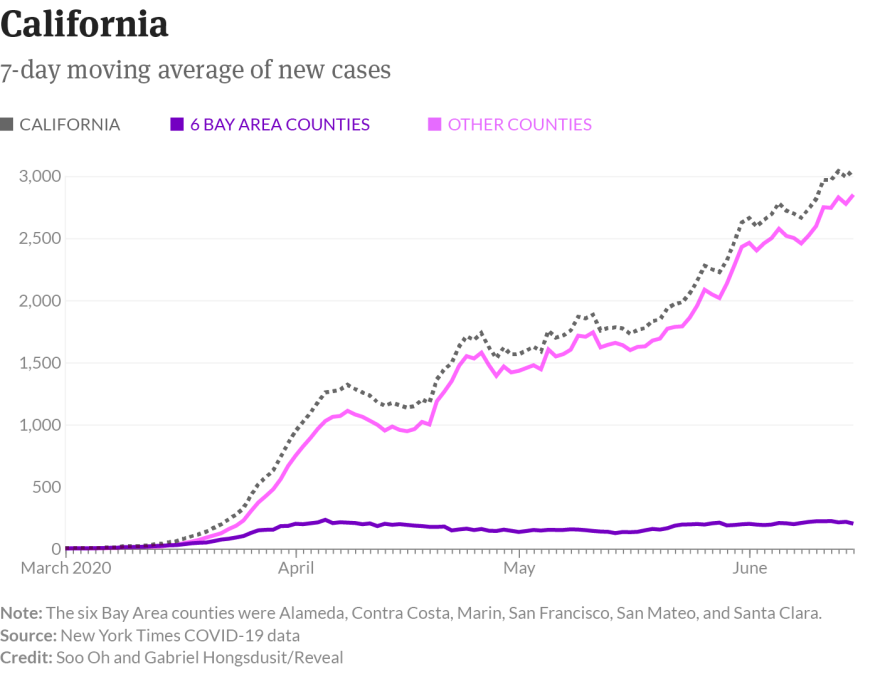
The same pattern was visible to a lesser extent in Florida, where officials in Miami-Dade and Broward counties mobilized quickly while Gov. Ron DeSantis embraced a laissez-faire approach. Just as in California, their decisions made a difference. By late April, confirmed cases in those counties began to drop as other Florida counties reported an increase.

Although the limited testing data makes it difficult to draw conclusions, the flattened curves in Florida and California “emphasize the point that early action makes a difference,” said Dr. Marissa Levine, director of the Center for Leadership in Public Health Practice at the University of South Florida. “In both states, we know that local leaders acted before state leaders did,” she said. “To some degree, we’re seeing that reflected in the data.”
By April 20, the day Florida’s task force for reopening first convened, California was reporting 86 cases per 100,000 residents, and Florida, 126. New York, the nation’s epicenter, had 1,293.
“Florida is not doing great,” Dr. John Swartzberg, the California epidemiologist, said in early May, before Florida began to reopen, “but it’s doing a lot better than I thought it would be given their really poor judgment, and a governor who doesn’t understand public health.”
But we may never know the full cost of DeSantis’ delays. Cellphone tracking data showed that Fort Lauderdale spring breakers dispersed to locales across the country, including to New York City, which would soon be overwhelmed. Nor can we know just how far the nation might have plunged into the COVID-19 abyss if California leaders had failed to take bold actions early on, clearing the way for elected officials elsewhere to follow suit.
“It was really critical to set a standard,” Levine said, referring to California. “Clearly, somebody had to go first. That always helps others make decisions a little more readily.” And California’s decision, she points out, built on Wuhan’s, where officials instituted a massive shutdown.
Ultimately, officials in both states faced dilemmas triggered by the lack of federal leadership – and the inability to conduct widespread testing. The testing shortage not only hampered early decision-making, but it also robbed local health officials of traditional tools such as testing and contact tracing and forced them to consider drastic, unprecedented measures such as shelter in place.
“The challenge we have here is that every state has kind of been left to its own to figure out the path forward,” Levine said. “To some degree, that’s OK. But it should be done under a national framework that provides some level of standardization.”
Such standardization would hinge on a strong testing infrastructure that, five months into the U.S. pandemic, is still not in place. Without it, states are still largely in the dark as they take steps to reopen.
Trump, resistant to aggressive testing from the start, has yet to embrace it as a linchpin of restarting the economy. Just three weeks after the U.S. became the global epicenter of the pandemic, the Trump administration released its guidelines for reopening, called “Opening Up America Again.”
That next week in Florida, DeSantis launched his Re-Open Florida Task Force. None of the executive committee members are medical doctors or epidemiologists. Instead, it’s packed with leaders of the state’s largest corporations. Thanks to their guidance, South Florida has begun to loosen restrictions, allowing businesses to open at a reduced capacity and reopening the beaches that are the engine of Florida’s tourism industry. Disney World plans to reopen next month. Schools may reopen in August.
As restrictions unravel, COVID-19 numbers have already begun to surge in Florida. On Thursday, the state recorded its highest number of reported cases in a single day.
Levine worries about the public abandoning safety measures as they emerge from strict shelter-in-place orders from the early days of the pandemic. “A lot of people think we did what we needed to do, and now we just need to go back to the way it was.”
“That’s the wrong message, unfortunately,” Levine said. “I think we may pay the price as we watch cases go up here in Florida and around the country.”
This story was edited by Esther Kaplan, Soo Oh and Matt Thompson and copy edited by Nikki Frick. Editors Terence Shepherd and Alicia Zuckerman from WLRN and Julia B. Chan and Ethan Toven-Lindsey from KQED contributed.
Follow or reach the reporters via email and Twitter. Lance Williams: lwilliams@revealnews.org and @LanceWCIR; Laura C. Morel: lmorel@revealnews.org and @lauracmorel; Marisa Lagos: mlagos@kqed.org and @mlagos; Caitie Switalski: cswitalski@wlrnnews.org and @caitielee0917; Melissa Lewis: mlewis@revealnews.org and @iff_or; Emily Harris: eharris@revealnews.org and @emilygharris.


